When we think of disease today what typically comes to mind is cancer, diabetes and heart disease. Seldom do we think about auto-immune diseases and especially neurological and mental health disorders. This article’s main concern will be on mental health and neurological diseases. A entire book can be written about this topic, however, this article will discuss:
- Current statistics regarding mental health disorders.
- What is the microbiome (gut bacteria) and what are its primary functions?
- Leaky gut, inflammation and its bio-markers that enter the bloodstream via the gut leading to poor brain function. Certain gut bacteria and its effects on healthy brain function.
- The relationship between the microbiome (gut bacteria), inflammation and mental health disorders like depression, anxiety/mood disorders, ADHD and autism.
- Things that make the gut go bad.
- Finally ways you can improve the gut that may lead to better brain health and/or a reduction in mental health symptoms.
This article is for information purposes and is not intended to replace treatment from a primary care physician or psychiatrist. In fact, any time you want to change your nutrition, you should inform your physician of these changes to ensure you will be safe from any adverse reactions that can occur mixing prescription drugs and foods/supplements. The main goal is to show you that the health of the gut does effect brain health and its proper function. There should not be a brain-body dualism anymore because neurosciences and modern medicine are showing that they are connected more so then we ever thought before.
- A 2013 British Report claims since 1979 there has been a 66% increase in brain diseases that leads to death.
- A 2013 report from the New England Journal of Medicine says we spend $50,000 annually caring for each dementia patient.
- America spends $200 billion per year treating dementia/Alzheimer disease. This is 2x’s what we annually spend on heart disease and close to 3x’s what we spend on cancer.
- 1 in 4 adults suffer from some kind of diagnosable mental health disorder.
- Anxiety disorders effect more than 40 million Americans.
- 10% of Americans have a mood disorder
- Depression effects 1 in 10 Americans. 25% of women in their 40’s and 50’s suffer from depression.
- Depression is the leading cause of disability worldwide and this diagnosis is growing.
- Prozac and Zoloft are among the most prescribed drugs in America today.

- People with bipolar and schizophrenia related disorders typically die 25 years earlier than the general population. This may be due to smoking, drinking and obesity, not just the strong drugs they are taking to control symptoms.
- Headaches and Migraines are the most common neurological disorders. 50% of Americans suffer from one or the other at least once a month.
- The National Pain Foundation claims that headaches and migraines account for 160 million lost work days in the U.S. and results in $30 billion a year in medical expenses.
- Multiple Sclerosis (an auto-immune disease) effect 2 1/2 million worldwide and 1/2 million in America. The average lifetime cost treating M.S. exceeds 1.2 million.
- Autism has increased 7 to 8x’s in the past 15 years.
Source of Statistics: Dr. David Perlmutter’s book “Brain Maker” Introduction and footnotes 3 through 10.
As you can see, mental health is effecting so many American individuals and families today. It is also hurting our economy, so we need to find ways to slow down the growing numbers at all cost. If not, America may experience a financial crises in the coming 20 to 40 years. I overheard this on C-Span back in 2015 where health professionals from the National Institute of Health and the Mayo Clinic were making this claim regarding the cost for the treatment of dementia alone.
Like I stated before, we must begin to realize that the brain and gut are intricately connected. The brain not only sends signals to the gut but the gut also sends signals to the brain. Science is now showing that brain health and brain diseases are dictated by what goes on in the gut. Science also affirms that up to 90% of all human illnesses are linked to an unhealthy gut.
The basic definition of the microbiome can be stated as “micro” for small and “biome” for a natural community of flora occupying a large habitat. In this case, it is your gut bacteria. Microbes out number the cells outside and inside our bodies. There are 10,000 species that have been discovered so far.  Each microbe contains its own DNA. Most of these microbes live in our gut. Every one of our cells is influenced by our microbiome and other organisms living in us. Your microbiome effects your mood, libido, metabolism, immune system, perception of the world, and even the clarity of your thoughts.
Each microbe contains its own DNA. Most of these microbes live in our gut. Every one of our cells is influenced by our microbiome and other organisms living in us. Your microbiome effects your mood, libido, metabolism, immune system, perception of the world, and even the clarity of your thoughts.
Scientific studies are continuing to show that the central nervous system, especially the brain is the most sensitive to changes in our microbiome. These bacterial DNA may have more of an impact on your health than your own genomics DNA. The microbiome may as well be considered an organ and scientists are calling this organ the “enteric nervous system.” This organ is just as important as your brain, heart, liver, lungs, etc. It communicates with the brain by sending signals through the “vagus nerve” the longest nerve of the cranial nerves. The microbiome or the enteric nervous system is created by the same tissue as the central nervous system in the growing fetus. Bacteria in the gut can release chemical messengers through the vagus nerve to the brain. The microbiome can function apart from the brain. This becomes important when it comes to mental health related issues as we will see later. Now that you know the basics of what the microbime is and its importance, let’s quickly discuss some of the functions of the microbiome.
Functions of Your Gut Bacteria
- Aids in digestion and the absorption of nutrients.
- Create a physical barrier against potential invaders such as bad bacteria (pathogenic flora), harmful viruses, and injurious parasites. Some types of bacteria have hair-like threads that help them swim; the “flagella,” as these threads are called, have recently been shown to stop deadly stomach rotavirus’ in its tracks.
- Act as a detoxification machine. The gut’s bugs have a role in preventing infections and serving as a line of defense against many toxins that make it down into your intestines. In fact, because they neutralize many toxins in your food, they can be viewed as a second liver. So when you decrease the good bacteria in the gut, you increase the workload of the liver.
- Profoundly influence the immune system’s response. Contrary to what you might think, the gut is your biggest immune system organ. Moreover, bacteria can educate and support the immune system by controlling certain immune cells and preventing autoimmunity (a state in which the body attacks its own tissues).
- Produce and release important enzymes and substances that collaborate with your biology, as well as chemicals for the brain, including vitamins and neurotransmitters.
- Help you handle stress through the flora’s effects on your endocrine-hormonal- system.
- Assist you in getting a good night’s sleep.Help control the body’s inflammatory pathways, which in turn effect the risk for virtually all manner of chronic disease.
All 8 points are from Dr. Perlmutter’s book, “Brain Maker,” pages 24 and 25.
Leaky Gut, Inflammation, Bio-markers, Gut Bacteria & Brain Function
The word “inflammation” comes from the latin verb “inflammare, which means to “kindle” or “to set on fire.” We hear about inflammation today and how it relates to diseases like cancer and heart disease but not enough about the role of inflammation and mental health disorders. Just like cancer and heart disease, mental health disorders like autism, depression, MS, Parkinson’s, Alzheimer’s, etc., are issues of chronic inflammation.
So are you telling me that the brain can have signs of inflammation? The answer is yes. However, the brain perceives pain from anywhere in the body but it does not have any pain receptors itself and cannot perceive that it is inflamed.
There are certain kinds of inflammatory bio-markers called cytokines that neuroscience is discovering that relates to brain inflammation and poor brain function. They are small proteins released by our cells that affect the behavior of other cells and take a primitive role in the inflammatory process. Cytokines like c-reactive protein (CRP), interlukin six (IL-6), and necrosis factor alpha (TNF-a). We now have the technology that can show these inflammatory biochemicals at work in the brain, the level of brain inflammation and the level of cognitive impairment.
Besides the inflammatory cytokines just mentioned, I would like to focus on LPS (lipopolysaccharides) to help you see the relationship between a leaky gut and inflammation in the brain. LPS is a combination of lipids (fat) and sugar and it is a major component of the outer membrane of certain gut bacteria. Without getting into too much detail what is important to state here is that LPS helps to sustain the integrity of the gut lining. However, once we compromise the gut lining with poor dietary habits, LPS can and does enter the bloodstream and causes inflammation to occur in the brain, leading to poor brain function that may cause symptoms related to numerous mental health disorders.
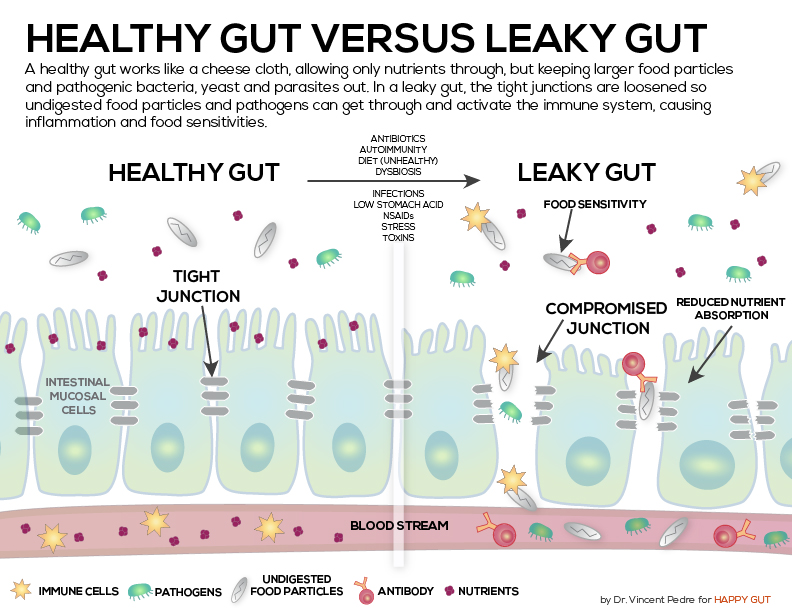 There are numerous things that lead to a leaky gut like too much sugar consumption, antibiotics, food allergies like gluten, prescription drugs, alcohol, refined foods, fried foods, etc. It has been shown in recent studies that those who have neurological disorders like Alzheimer’s disease, multiple sclerosis (MS), Parkinson’s disease, amyotrophic lateral sclerosis (ALS), depression and even autism have high levels of LPS in their bloodstream.
There are numerous things that lead to a leaky gut like too much sugar consumption, antibiotics, food allergies like gluten, prescription drugs, alcohol, refined foods, fried foods, etc. It has been shown in recent studies that those who have neurological disorders like Alzheimer’s disease, multiple sclerosis (MS), Parkinson’s disease, amyotrophic lateral sclerosis (ALS), depression and even autism have high levels of LPS in their bloodstream.
High levels of LPS in the bloodstream is also a bio-marker of a “leaky gut.” In fact, it is not uncommon for people with mental health disorders to have multiple gut related diseases. High levels of LPS may cause memory problems as well. Dr. Christopher Forsyth of Rush University Medical Center in Chicago has explored LPS and its relation to leaky gut (or gut permeability) that is linked to Parkinson’s disease and has found a direct correlation. His patients with Parkinson’s disease in his study shows higher amounts of LPS in the bloodstream than the healthier controls. As you can see, there is a direct correlation between gut permeability, inflammation and brain permeability that can lead to symptoms related to mental health disorders.
I would like to briefly discuss the role of gut bacteria/microbiome in manufacturing certain types of brain chemicals to help sustain a healthy more functional brain.
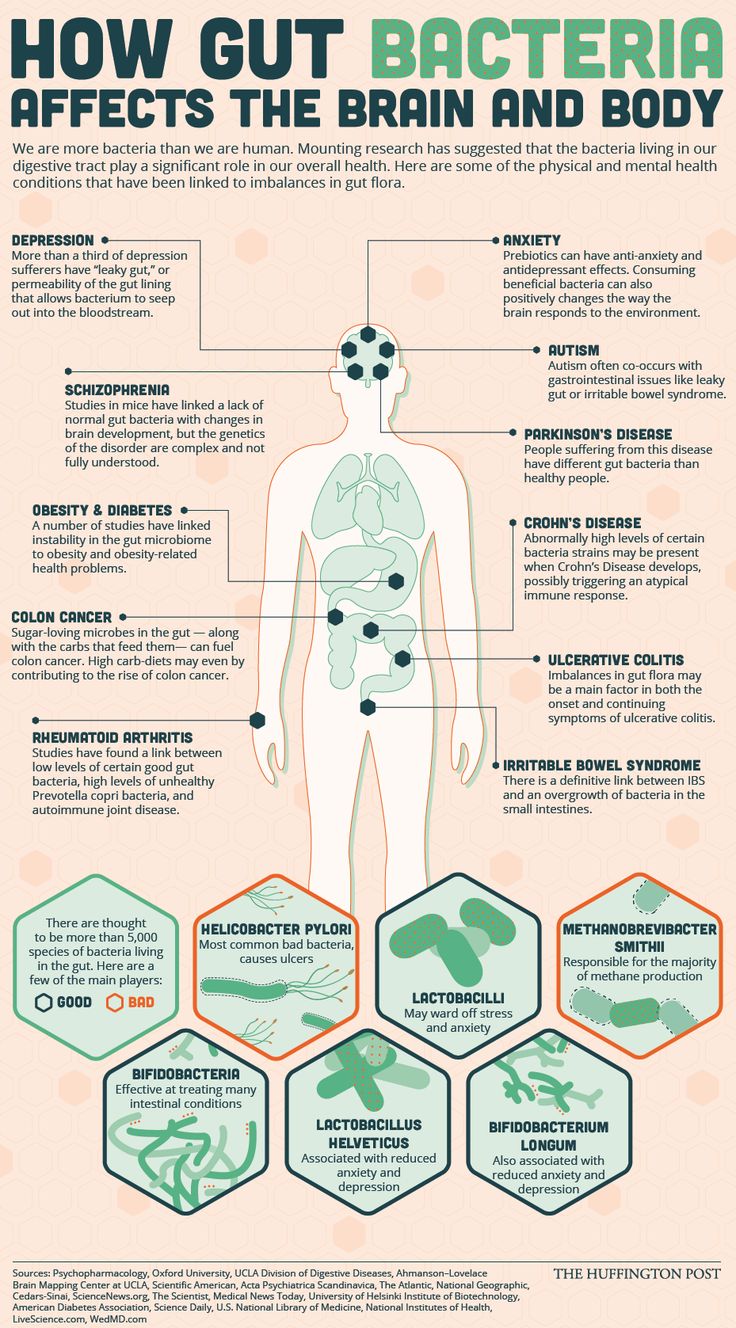
The first is called, “BDNF” (brain derived neurotrophic factor) that is a critical brain growth protein. It is involved in neurogenesis, protecting existing neurons, and encourages new connections between new and old neurons. Low levels of BDNF are found in mental and neurological disorders like Alzheimer’s, epilepsy, anorexia nervosa, depression, schizophrenia and OCD (obsessive compulsive disorder). Having a healthy gut will enable you to produce adequate amounts of BDNF to ensure you maintain a healthy brain.
 The second is called, “GABA” (gamma amino butyric acid). GABA is an amino acid that serves as a neurotransmitter in central nervous system. It helps to calm nerve activity. A particular strain of bifidobacterium secretes large amounts of GABA that can help to control anxiety type disorders and even anxiety related gut disorders like Crohn’s disease. Any leakiness of the gut mentioned above will hinder the production of GABA that could make it harder to control anxiety problems.
The second is called, “GABA” (gamma amino butyric acid). GABA is an amino acid that serves as a neurotransmitter in central nervous system. It helps to calm nerve activity. A particular strain of bifidobacterium secretes large amounts of GABA that can help to control anxiety type disorders and even anxiety related gut disorders like Crohn’s disease. Any leakiness of the gut mentioned above will hinder the production of GABA that could make it harder to control anxiety problems.
Lastly, the amino acid “glutamate.” This amino acid neurotransmitter is produced by your gut bacteria that assists in cognitive function, learning and memory.
This section has taught you how a leaky gut leads to systemic inflammation and how certain bio-markers are released in the bloodstream causing symptoms of mental and neurological pathology and overall poor brain function. You have also learned briefly how healthy gut bacteria produces amino acid neurotransmitters to help produce a healthy brain. We now know that other neurotransmitters like dopamine, serotonin and many others are produced by a healthy gut that assists in better brain function and you will see more of this as we move along in the article. I hope it is becoming clear that the gut has a huge impact on your mental health and how the brain-gut dualism is no longer a sustainable belief.
Depression
It is mind blowing to know that 30 million Americans were prescribed anti-depressants in 2014 that totaled $12 billion dollars worth. America is spending more on anti-depressants then the Gross National Product of more than half of the world’s countries. SSRI’s (selective serotonin re-uptake inhibitors) prescribed to treat depression has increased 400% in the last 20 years. Back in 2005 anti-depressants were the #1 prescribed drug in the U.S. Drugs like Prozac, Cymbalta, Zoloft, Elavil, Lexapro and Wellbutrin. I have personally seen what depression does to people working at a mental health facility for 8 years now. Many of these drugs seem to work for some but for many others they try numerous ones and show little to no improvement. The pharmaceutical industry knows that inflammation is part of the problem with depression so many of these drugs may impact inflammatory markers in the body more so than actually working on brain chemicals like serotonin to help alleviate symptoms of depression. However, these drugs take a toll on the microbiome and may cause gut related side effects. In fact, some people have never dealt with depression until their gut issues started for various reasons.
Back in 1933, A. Ferrao and J.E. Killman published a paper in the journal of Psychiatry titled, “Experimental Toxic Approach to Mental Illness,” and in this paper they state, “It is far from our mind to conceive that all mental conditions have the same etiological factor, but we feel justified in recognizing the existence of cases of mental disorders which have as a basic etiological factor a toxic condition arising in the gastrointestinal tract.” When this study came out, it was at a time when the scientific community failed to see that the gut’s influence on the brain is crucial to mental health disorders. The scientific community only saw that the brain influences the gut and avoided these early findings that the gut influences the brain just as much.
Well we now know that the microbiome and inflammation has a lot to do with depression. In 2011, a study that was done at McMaster University in Ontario, Canada was the first to really show how the gut can really influence the brain and brain behavior. This study came out 78 years after the 1933 study came out but it has more bearing on the scientific community today since the study of the microbiome is being looked at with greater concern as it pertains to mental health disorders.
So what inflammatory markers can we measure that effect depression? It has been shown that high levels of LPS in the bloodstream effect the level of depression in individuals (see “Brain Maker” ch. 3 note 20 in bibliography for reference). Foods that are high in glycemic and high fructose corn syrup increase inflammatory markers like c-reactive protein and LPS in the bloodstream and pass the blood-brain barrier causing symptoms of depression.
So you can see that high blood sugar increases the chances of depression and worsens depression. It is safe to say that depression is an inflammatory disease that may be caused by dysbiosis (imbalance of healthy gut flora) in the microbiome. I am not saying the sole cause of depression is poor gut health but is a potential cause of depression and high levels of LPS in the bloodstream is just one indicator of this reality.
To give you one example of how gut bacteria produces brain like neurotransmitters that may help treat depression, let’s look at bifidobacterium infantis. This particular probiotic makes trytophan in the gut. Trytophan is important because it is a precursor of serotonin that is also produced in the gut. These two neurotransmitters produced in the microbiome can potentially decrease depression, so long as, we eliminate the systemic inflammation caused mainly by dietary choices. I will discuss others things that lead to an unhealthy gut and ways to improve gut health in section five and six. For now, let’s turn to anxiety/mood disorders.
Autism
The United Nations estimates that 70 million people worldwide fall under the autism spectrum; 3 million of them live in the U.S. 1 in 68 American children are currently on the autism spectrum. This is a 10-fold increase in the past 40 years. This means that 1 in 42 boys and 1 in 189 girls are diagnosed with some form of autism. Some doctors argue that this is because of better diagnostic capabilities which may be the case but other doctors put the blame on lifestyle related practices that effect the gut and other biological and biochemical pathways. The most common symptoms range from difficulties in social interaction, challenges in verbal and nonverbal communication and repetitive behavior.
Most children with autism have GI issues like abdominal pain, constipation, diarrhea, bloating, etc. In 2012, the National Institute of Health evaluated autistic children and found that 85% were constipated and 92% had some form of GI issue(s). In fact, in October of 2005 the Journal of Medical Microbiology published a study titled, “Differences between the Gut Microflora of Children with Autistic Spectrum Disorders and That of Healthy Children,” showing clear a distinction between the microbiome of both groups.
Those who had some form of autism had high levels of clostridial species and less beneficial bacteria like bifidobacteria. This may give us an explanation as to why autistic children crave carbohydrates. The most famous of the clostridial species is C. diff. This overgrowth in the autistic child’s gut is more than likely caused by antibiotic use. High levels of clostridial bacteria produces high levels of propionic acid and this enters the bloodstream and harms the brain. The gut bacteria in autistic children create compounds that are harmful to their immune system and brain. Their microbiome triggers the immune system, as a result, this increases inflammation in the bloodstream causing harmful inflammatory chemicals to enter the brain and alter mood and neurological function. There are high levels of LPS in the bloodstream as well in autistic children. Scientists still do not know if gut bacteria is a cause or effect of autism but scientific studies show that getting the microbiome healthy reduces symptoms.
This section would not be fair if genes were not a topic of discussion. Genes are a factor as well when it comes to autism. Scientists have discovered as many as 100 genes that change/mutate during fetal development that are associated with autism. There can also be mutations that occur in the egg or sperm before conception, so autism may not always be connected to the mother or father. Many scientists and doctors do attribute autism to gene and environmental factors. The complexity of this neurological and behavioral disorder does not exempt one or the other.
There are physicians who are utilizing oral probiotics as a part of the nutritional treatment for autistic children and are having some success. Plus, the elimination of refined carbohydrates, gluten, food colorings and additives, fried foods, any refined oils, fructose like high fructose corn syrup, GMO foods, all forms of refined sugar, pasteurized dairy products, etc., will possibly reduce symptoms as well since all these listed cause inflammation. The complexity of this disorder has to include more than probiotic use but that goes beyond the scope of this article.
Anxiety/ Mood Disorders
Anxiety and mood disorders effects 40 million Americans per year. These disorders range from GAD (general anxiety disorder), panic disorder, OCD (obsessive compulsive disorder) and social phobias. Like depression, when the gut is in a dysbiotic state, this causes high levels of systemic inflammation that enter the bloodstream through the gut lining. There has been studies showing that those with anxiety and mood disorders have low levels of BDNF in the hippocampus, high levels of cortisol and an overreaction stress response that leads to gut permeability (aka leaky gut). The microbiome that is unhealthy and dysbiotic effects immune function, hormone function and neurological function. As a result, you may be less likely to handle stress which may cause some anxious or mood related symptoms.
There was a study done in 2015 at the University College Cork titled, Mind-Altering Probiotic Bacteria May Lessen Anxiety and Depression,” which gives us an indication that anxiety and mood disorders may be directly related to the health of our microbiome. There was a prebiotic study done at the University of Oxford by neurologists back in 2015 showing that prebiotics (food for healthy probiotics) may help alleviate anxiety by reducing the amount of cortisol in the bloodstream. Having a healthy microbiome can and does influence our reaction to outside stimuli whether it be good or bad according to these Oxford University neurologists.
People who have anxiety and/or mood disorders show low levels of trytophan production in the gut which is produced by the bacteria bifidobacterium infantis. These low levels of trytophan increase the by-products of broken down tryptophan called, “kynurenine.” Elevated levels of kynurenine has been associated with anxiety, depression, alzheimer’s, cardiovascular disease and even tics. Bifidobacterium infantis has been shown to calm down the stress response because it lowers levels of kynurenine. With lower levels of kynurenine then there is more tryptophan available to be used for the production of serotonin, this is important for preventing symptoms of depression and anxiety. There are numerous neurologists and other general medical practitioners who hope that probiotic therapy will be a part of treating mental health disorders.
ADHD
More than 11% of children between the ages of 4 to 17 are diagnosed with ADHD and are put on drugs like Ritalin and Adderall or non-stimulant drugs like Strattera. There are more than 10,000 American toddlers between 2 and 3 years old being treated for ADHD. This is extremely early to make such a diagnosis at the toddler age but it is going on and quit honestly it is a form of malpractice in my opinion. Neurologists still do not know the long-term effects of these drugs on brain development.
In 2000, a study that was published by the American Journal of Clinical Nutrition that was carried out by Dr Laura Stevens of Purdue University reveals some interesting facts about the risk of ADHD in children. She reveals that there is a direct relationship between how long a child is breast-fed and the risks of becoming ADHD. She also discovered that children who have numerous ear infections and are treated with antibiotics was associated with a greater risk of becoming ADHD. This does not mean that this will occur in all children but we know what antibiotics do to the microbiome! Antibiotics change the bacterial environment of the gut, increase gut permeability and increase inflammatory markers in the blood that break the blood-brain barrier where these inflammatory chemicals effect brain function. The longer a mother breast feeds her newborn, the more their intestinal tract will be populated with healthy gut flora, boost their immune system and reduce chances of many illnesses in the future, including ADHD.
Children with ADHD have many digestive problems like constipation and some have what is called “fecal incontinence” (losing control of the bowels). Some German scientists have shown a connection between gluten sensitivity and ADHD symptoms. They recommend testing for gluten sensitivity as a part of the evaluation process for ADHD. Many of us now know the effects of gluten in the gut and its inflammatory effects that can cause someone to develop gut disorders. Not only gluten but also dairy, processed foods and food colorings can also cause symptoms of ADHD. They all can lead to gut permeability and inflammation in the bloodstream wreaking havoc on brain function.
Dr. Richard Edden, an associate professor of Radiology at John Hopkins University School of Medicine used a magnetic resonance spectroscopy that allowed him to measure chemicals in humans. What he discovered was low levels of the amino acid neurotransmitter GABA in ADHD children. Remember that this amino acid can be produced by certain strands of gut bacteria, especially strands of the lactobacillus and bifidobacterium groups (especially lactobacillus helveticus and bifidobacterium longum). Once again, you see how the microbiome and its healthy environment can help to produced certain amino acid neurotransmitters needed for proper brain function and this is produced more so in the gut than the brain. Over time, I believe you will see doctors use prebiotics and probiotics as a part of the medical treatment for mental health disorders as more and more studies confirm their efficacy in treatment.
AVOID THE FOLLOWING:
| Refined Sugar | Alcohol | Artificial Sweeteners |
|---|---|---|
| Antiobiotics | Prescription Drugs | C Section/Formula Babies |
| GMO Foods | Gluten & Dairy | Fructose/HFCS |
| Enviromental Chemicals | Refined Oils | Cigarettes & Illegal Drugs |
| Processed Foods |
Negative Thoughts |
Sport & Carbonated Drinks |
The list goes on and on but I think this is a good list. It covers a lot of areas to consider. The goal is to minimize our exposure to most of these but complete avoidance is near impossible. For women who may be reading this, if you had a c-section and formula fed your child/children, do not worry or feel bad. If you find yourself eating lots of these foods it’s alright. The good news is what we are going to turn to next. The good thing is that our bodies can regenerate after years of abuse. For many of us, we did not know all these factors can influence our microbiome that may lead to mental health disorders. So how can you regenerate your microbiome and/or your child/children’s’ microbiome?
- Daily pH stabilized Probiotics like Digestive Health (also included in our unique formula is prebiotics and broad spectrum digestive enzymes)
- Superfoods like in Core Greens (easiest) or increase dark leafy greens intake (spinach, kale, mustard greens, etc.)
- Good fats, especially omega 3 fatty acids like Core EFAs and add raw nuts, seeds, organic cold pressed flax oil, chia seeds, coconut oil and avocados to your diet.
- Ionized Kangen Water (electrically charged water has been shown in the Japanese medical literature to help proliferate good gut flora)
- Organic coffee (limit to a few cups per day). Try our cold brew recipe with Kangen water or choose organic green tea!
- Organic dark chocolate (2 to 3 pieces per day)- look for lowest amount of sugar
- Organic fermented foods and drinks rich in probiotics (lacto-fermented sauerkraut, kimchi, kombucha tea, kefir, pickles, and cultured condiments)
- Organic Raw Apple Cider Vinegar (“with the mother”-a great prebiotic)
- Raw honey (local is best)
- Prebiotics like Granny Smith apples, artichokes, raw garlic, raw onions, acacia gum, raw chicory root, raw Jerusalem artichoke, raw dandelion greens, raw leeks, cooked onion or lightly steamed asparagus
- Positive thoughts and daily affirmations
- Sunshine and aerobic exercise (daily)
- Clean protein- wild caught fish or grass-fed beef (don’t forget your digestive enzymes to increase the utilization of that protein)
Check out this great article 12 Gut Cleansing Foods to Include in Your Diet. If you begin to implement these amazing foods and nutritionals plus eliminate the negative dietary habits, you will be on your way to better gut health. Your microbiome and your brain will thank you! Remember, the complexity of mental health disorders need a plethora of nutritional intervention but this is a great start. I could have discussed heavy metal toxicity, nutrient deficiency, nutrient toxicity, yeast/fungal overgrowth, hyper/hypothyroidism and many other areas regarding its effects on mental health but this article’s focus was just on the connection of the microbiome and the brain. All the advice given in this article is not intended to treat or diagnose mental health diseases. Please be under the care of a physician while making any dietary changes. If you are currently taking psych medications, please consult your physician or pharmacist to ensure no adverse reactions can occur implementing these foods while taking your medications. It is my hope that you or someone you know may experience an improvement in your mental health!

To life, health, longevity and happiness!!
John Nardozzi
Enzyme Nutritionist & Blog Writer
Bibliography
Perlmutter, David, MD. The Brain Maker: The Power of Gut Microbes to Heal and Protect Your Brain-For LIfe. New York, NY. Little Brown and Company. 2015.
K.M. Neufeld et al., “Reduced Anxiety-like Behavior and Central Neurochemical Change in Germ-Free Mice,” Neurogastroenterol. Motil. 23, no. 3 (March 2011): 255-64.
M. Maes et al. “The Gut-Brain Barrier in Major Depression: Intestinal Mucosal Dysfunction with an Increased Translocation of LPS from Gram Negative Entero-bacteria (Leaky Gut) Plays a Role in the Inflammatory Pathophysiology of Depression,” Endocrinol. Lett. 29, no. 1 (February 2008): 117-24.
A. Ferrao and J. E. Kilman, “Experimental Toxic Approach to Mental Illness,” Psychiatr. Q. 7 (1933): 115-53.
Maria Almond, “Depression and Inflammation: Examining the Link,” Curr. Psychiatry 6, no. 12 (2013): 24-32
“Depression (Major Depressive Disorder): Selective Serotonin Reuptake Inhibitors (SSRI’s),” http://www.mayoclinic.org/disease-conditions/depression/in-depth/ssris/art-20044825.
University College Cork, “Mind-Altering Microbes: Probiotic Bacteria May Lessen Anxiety and Depression.” Science Daily, 2011.
K. Schmidt et al., Prebiotic Intake Reduces the Waking Cortisol Response and Alters Emotional Bias in Healthy Volunteers,” Psychopharmacology (Berl.) (December 3, 2014).
Bested et al., “Intestinal Microbiota,” Part II.
J.R. Burgess et al., “Long-chain Polyunsaturated Fatty Acids in Children with Attention-Deficit Hyperactivity Disorder,” American Journal of Clinical Nutrition. 71, Suppl. January 2000, 327S-30S.
H. Niederhofer, “Association of Attention-Defecit/Hyperactivity Disorder and Celiac Disease: A Brief Report,” Prim. Care Companion CNS Disord. 13, no. 3 2011.
E. Barrett et al., “G-Aminobutyric Acid Production by Culturable Bacteria from the Human Intestine,” Journal of Applied Microbiology. 113, no. 2 August 2012, 411-17.
J Luo et al., “Ingestion of Lactobacillus Strain Reduces Anxiety and Improves Cognitive Function in the Hyperammonemia Rat,” Sci. China Life Sciences 57, no. 3 March 2014
M. Messaoudi et al., “Assessment of Psychotropic-like Properties of a Probiotic Formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in Rats and Human Subjects,” British Journal of Nutrition, 105, no. 5, March, 2011.
Melinda Wenner Moyer, “Gut Bacteria May Play a Role in Autism,” Scientific American Mind 25, no. 5, August 14, 2014.
J.F. White, “Intestinal Pathophysiology in Autism,” Exp. Biol. Med. Maywood 228, no. 6, June 2003: 639-49.
J. G. Mulle et al., “The Gut Microbiome: A New Frontier in Autism Research,” Curr. Psychiatry Rep. 15, no. 2, February, 2013: 337.
S.M. Finegold et al., “Gastrointestinal Microflora Studies in Late-Onset Autism,” Clin. Infect. Dis. 35, Suppl. 1, September, 2002: S6-S16.
Parracho et al., “Differences between the Gut Microflora.”
P. Gorrindo et al., “Gastrointestinal Dysfuction in Autism: Parental Report, Clinical Evaluation and Associated Factors,” Autism Res. 5, no. 2, April, 2012: 101-8.
Sarah Deweerdt, “New Gene Studies Suggest There Are Hundreds of Kinds of Autism,” Wired, November 25, 2014.
“Scientists Implicate More Than 100 Genes in Causing Autism,” NPR, October 29, 2014.
[/fusion_text]



[…] take steps toward improving the bacteria in your gut and decrease stress and other ailments head to Core Health and learn […]
Thanks, Shan for your wisdom!
This is amazing and came just at the right time for me. Thanks!